· Michele Mazzucco · Post · 8 min read
When waiting becomes the problem — why healthcare can’t afford to stand still
In healthcare, even a single minute can make a meaningful difference. Yet patients are waiting not just minutes, but weeks or months — and the hidden costs ripple far beyond the waiting room.

Image from freepik
In healthcare, waiting is more than just a waste of time — it can have real, lasting consequences. Long wait times have become commonplace around the world — and the cost is rising. Many see these delays as inevitable in an overburdened system, rather than a problem that can be solved.
Waiting costs more than just time and patience. It affects everything — how well patients recover, how providers work, how quickly staff burn out, and how resources get misused in the system. And while there is no silver bullet, there are sustainable ways to reduce the burden.
Table of contents
- The global scope of the problem
- What delays in care cost
- Why quick fixes aren’t enough
- What can be done: practical moves that matter
- Real change, without the waiting
The global scope of the problem
Patients everywhere are sitting around longer to get care — and they have started to notice.
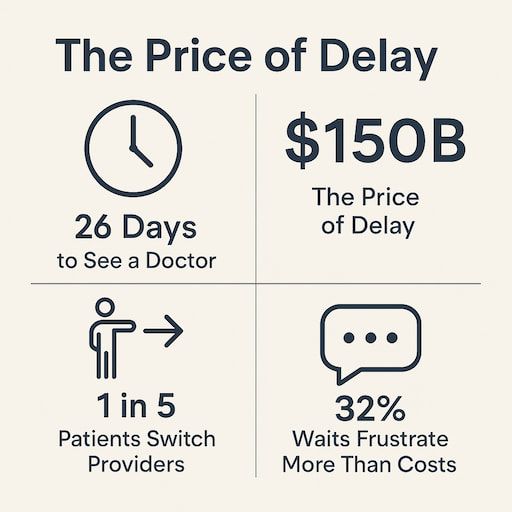
- A Bain & Company study found that wait times now frustrate patients more than out-of-pocket costs, particularly in primary and specialist care.
- In the U.S. new patient wait 26 days for a primary care doctor, which is a 24% increase compared to 2004.
- Across OECD countries, waiting for surgery or specialist appointments is still a major issue. Median wait times for elective surgeries range between 30 and more than 120 days varying by country.
These delays are not just statistics. They lead to missed diagnoses slow treatments, and rising stress for both patients and healthcare providers.
What delays in care cost
When someone visits a healthcare facility, they expect fast and compassionate care. Long waits, unfortunately, often bring more problems than people realize. These delays can hurt patients’ health, strain a clinic’s finances, and damage how much faith people have in their healthcare providers. The impact goes much deeper than just overcrowded waiting areas.
Loss of patient trust and satisfaction
Picture walking into a clinic already worried about your health to sit for hours waiting your turn. This isn’t just annoying — it can make you question the entire healthcare system. Long wait times can leave patients feeling ignored or less important, which might break their trust in their caregivers.
Damaged trust leads to deeper consequences:
- Patients may delay or avoid seeking future care, risking worse health outcomes.
- Frustrations are often shared widely, eroding community trust and tarnishing reputations.
- The doctor-patient relationship suffers, impacting continuity and quality of care.
Reducing wait times shows patients something important. It says, you matter and your time is important. Recently, I experienced firsthand the hidden cost of long healthcare delays through a family member’s situation. After being referred for a critical consultation, days turned into weeks with no clear updates. Each call to the clinic was met with a vague, “We’ll let you know,” offering little reassurance and no real timeline. The waiting wasn’t just inconvenient — it was emotionally draining. The uncertainty bred deep frustration and a painful sense of being forgotten, of being “just another number” in a crowded system.Personal reflection
It was a powerful reminder that delays don’t only affect health outcomes; they erode trust, dignity, and peace of mind. Behind every delay is a person simply hoping to be seen, heard, and cared for.
How long wait times affect patients’ health
Delays in care can hurt a patient’s health. For example, a recent study found a clear link between long waits and poorer clinical outcomes in public health systems.
Extended delays in receiving care can result in:
- Delays in spotting and treating illnesses, especially those cases that demand quick care.
- Rising stress and worry levels, which can slow down healing.
- Worsening health problems, as untreated issues may get more severe.
To manage symptoms and avoid complications in long-term illnesses, acting promptly really matters. Cutting down on long waits allows doctors to start care earlier helping many patients recover better as time goes on.
Financial strain on healthcare providers
Beyond the human impact, long wait times can significantly hurt the financial health of healthcare providers. Dissatisfied patients don’t just leave emotionally — they often take their business elsewhere. This can lead to:
🗓️ Loss of repeat business
Regular patients who experience long wait times may switch to another provider.
🤐 Reduced referrals
Dissatisfied patients are less likely to recommend services to friends and family.
📉 An overall drop in revenue
Fewer patients and lower patient loyalty can hurt the bottom line.
The cumulative impact is staggering. Missed or delayed appointments contribute to an estimated $150 billion in lost revenue annually in the U.S., according to Phreesia. Longer wait times create a vicious cycle: lost revenue limits a facility’s ability to invest in solutions — which only worsens the problem.
The toll on staff and operational efficiency
It is worth noting that there is a team working behind every crowded waiting room. Long waits do not just frustrate patients; they also put pressure on the staff. Packed schedules and ongoing inefficiencies create challenges that affect healthcare workers in many ways, including:
🤯 Staff stress and burnout rise
Handling irritated patients drains energy from the team
😞 Lower morale
When employees see that their hard work is not translating into positive patient experiences, their motivation can decline.
🚧 Operational disruptions
Inefficient systems can lead to disorganization, making it harder for staff to manage appointments and provide timely care.
Why quick fixes aren’t enough
It is important to recognize that there is no quick fix to this problem. Healthcare systems worldwide are dealing with rising costs and shrinking resources. Immediate and cheap solutions are, frankly, unrealistic.
Adding more staff or constructing new facilities can be helpful, but those are strategies that take time. The more immediate opportunity lies in improving flow—making the most of the resources that already exist.
What can be done: practical moves that matter
Cutting down wait times isn’t just about vague improvements — it takes deliberate actions that change daily operations. Here are key strategies that drive real impact:
🏎️ Streamline patient flow — by identifying and removing bottlenecks
Instead of simply telling staff to “work faster,” map out every step from check-in to discharge.
- Action: use time-motion studies or even simple observation logs to spot where patients queue unnecessarily — like at registration, outside imaging, or waiting for paperwork.
- Concrete fix: adjust staff assignments during peak hours, add mobile check-in, or use clear wayfinding to prevent backtracking and confusion.
🚀 Maximize scheduling efficiency — with demand-based booking
Most wait times balloon due to mismatches between patient demand and available slots.
- Action: analyze appointment data to identify busy vs. slow times.
- Concrete fix: shift from “first come, first served” to “appointment blocks” for different needs — e.g., rapid slots for bloodwork, longer slots for new consults. Use automated reminders to reduce no-shows.
🛏️ Unlock ambulatory and outpatient capacity — with parallel processing
Ambulatory Surgery Centers (ASCs) and outpatient clinics face unique pressures to maintain high-volume, high-speed care. Instead of one-at-a-time, find steps that can overlap safely.
- Action: let patients fill out intake forms and pre-op checks simultaneously, rather than waiting for each step in sequence.
- Concrete fix: create a “prep zone” where multiple patients are readied at once, or batch similar procedures to minimize turnaround time between cases.
🔬 Enhance diagnostic and lab turnaround — with real-time communication
Delays often occur when test results are “stuck” waiting to be noticed. In the worst case scenario, this may even cause the re-planning of entire treatments.
- Action: implement automatic alerts for completed results sent directly to clinicians, reducing idle “queue time.”
- Concrete fix: set daily cut-off times for sample pick-ups or use color-coded dashboards to flag urgent tests, so nothing sits unnoticed at the back of the line.
📱 Make telehealth work — by managing digital queues
Virtual visits help, but only if the digital “waiting room” is managed properly.
- Action: use virtual queue systems that show patients their expected wait time and allow them to complete forms in advance.
- Concrete fix: allow patients to receive texts when a provider is ready, minimizing on-screen waiting and improving satisfaction.
💡 Professional note: these are the kinds of changes we specialize in — sometimes as simple as a new checklist, sometimes involving technology or workflow redesign. Our experience optimizing complex queues in other industries gives us a proven toolkit for tackling healthcare’s unique challenges.
The key is measuring the impact: before and after times, patient feedback, and fewer bottlenecks you can see in action.
🔍 Measuring what matters: predict, don’t just react
Real change, without the waiting
In a world where every minute matters, understanding — and acting on — the hidden costs of long patient wait times is essential. Solving these challenges takes more than promises or quick fixes. Lasting progress comes from practical steps: measuring what’s really happening, modeling the impact, and making smart, targeted changes to workflows and queues.
The truth is, patient wait times won’t disappear overnight. But meaningful improvements are always possible. By focusing on the right details, healthcare organizations can reduce frustration, smooth out the patient journey, and give both patients and staff a better experience — without expensive overhauls or unrealistic expectations.
At its core, modern queue and workflow optimization is about removing obstacles, not chasing miracles. That is where real progress begins.
📬 Get weekly queue insights
Not ready to talk? Stay in the loop with our weekly newsletter — The Queue Report, covering intelligent queue management, digital flow, and operational optimization.



